by Lexington Vein Institute | Jun 8, 2021 | Blog, Varicose Veins
Chronic Venous Insufficiency (CVI) is an issue that affects about 40 percent of the US population. It’s often overlooked by healthcare providers. It can present itself as other venous disorders.
Read on to learn more about this disease and your treatment options.
Chronic Venous Insufficiency
What is Chronic Venous Insufficiency (CVI)? CVI is a condition in the veins that allows blood to flow back to the heart. The valves in the deep veins of the leg do not properly work and the blood flows backward.
This causes the pooling of blood in those veins. CVI is not a serious health emergency but it can be painful.
Symptoms
It’s important to contact your healthcare provider if you have any of these symptoms. Without treatment, this disease can cause more serious issues.
Symptoms to look for are:
- Any swelling in the legs or ankles
- Pain when walking
- Leg cramps or a tight feeling in your calves
- Brown or leather looking skin
- Varicose veins or leg ulcers
- Restless leg syndrome or leg itchiness
Any of these symptoms by themselves doesn’t mean you have CVI. A combination of them could be a sign to visit the doctor. This is particularly important if you are at a higher risk for the disease.
Causes
There are a few causes that professionals believe cause CVI.
If you’ve had deep vein thrombosis, a previous injury, or surgery, you’re at a higher risk to develop the issue.
Those that don’t get enough exercise or who sit or stand for a long period, are also at a higher risk. Smokers also tend to develop CVI more than non-smokers.
If you are overweight or pregnant you’re at a higher risk, as are those with a family history.
Phlebitis is also a known risk factor.
Women are more likely than men to have a diagnosis of CVI.
The good news is the medical field has developed ways to treating this issue.
Diagnosis
Your healthcare provider will go over your medical history and do a full examination.
The doctor may order a Duplex ultrasound done, which checks the blood flow in the leg. It also can see the speed and direction of your blood flow.
Make sure you’re honest with your physician when going in for a diagnosis.
Treatments
CVI is most treatable in its early stages. Your healthcare provider may recommend a combination of therapies. This is depending on the severity and medical history.
Your doctor might first recommend a moisturizing routine to help treat VCI. Moisturizing helps skin from flaking or cracking.
Your doctor may also recommend compression stockings. They put pressure on the legs that aids in blood flow.
Exercise is a great and preferred method of treatment because it keeps blood flowing. Walking is also good if you need low-impact exercise.
You should try not to sit or stand for long periods of time. If you have to sit for long periods, make sure to wiggle your legs to keep blood flowing. If you must stand for long periods, take breaks and elevate your feet.
Your doctor may also prescribe an antibiotic if you have an infection from leg ulcers.
Advanced Treatment Options
If you have an advanced case of VCI, your doctor may want to use a more advanced method of treatment.
Sclerotherapy is a procedure that injects a solution into the vein and causes scarring. This makes the blood flow stop and will flow through other veins.
Your physician may also want to try Endovenous Thermal Ablation. This uses high-frequency radio waves that heat and close the vein.
A ligation is also an option. This is when a surgeon cuts and ties off the vein to stop blood flow. They will also remove the vein if it’s damaged.
Finally, they may want to use a small incision that removes the vein. This procedure is known as an Ambulatory Phlebotomy.
Remedy CVI
If you think you have CVI or have already been diagnosed treatment will help. Dr. Fadi Bacha has helped patients like you live their best lives for the past 10 years. Contact the Lexington Vein Institute today for a treatment plan for you.

by Lexington Vein Institute | Jun 8, 2021 | Blog, Varicose Veins
One in three Americans over the age of 45 have some form of vein disease. Many are unaware, while others view the symptoms as minor; however, vein disease must be taken seriously due to the veins’ integral role in blood supply and flow.
What is Vein Disease
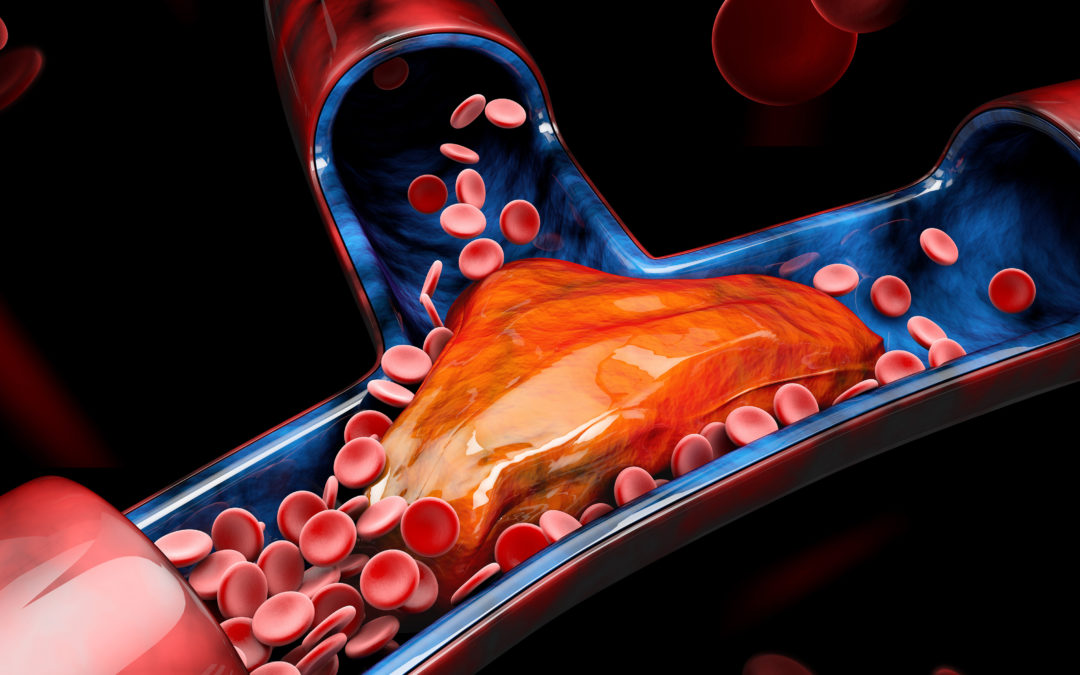
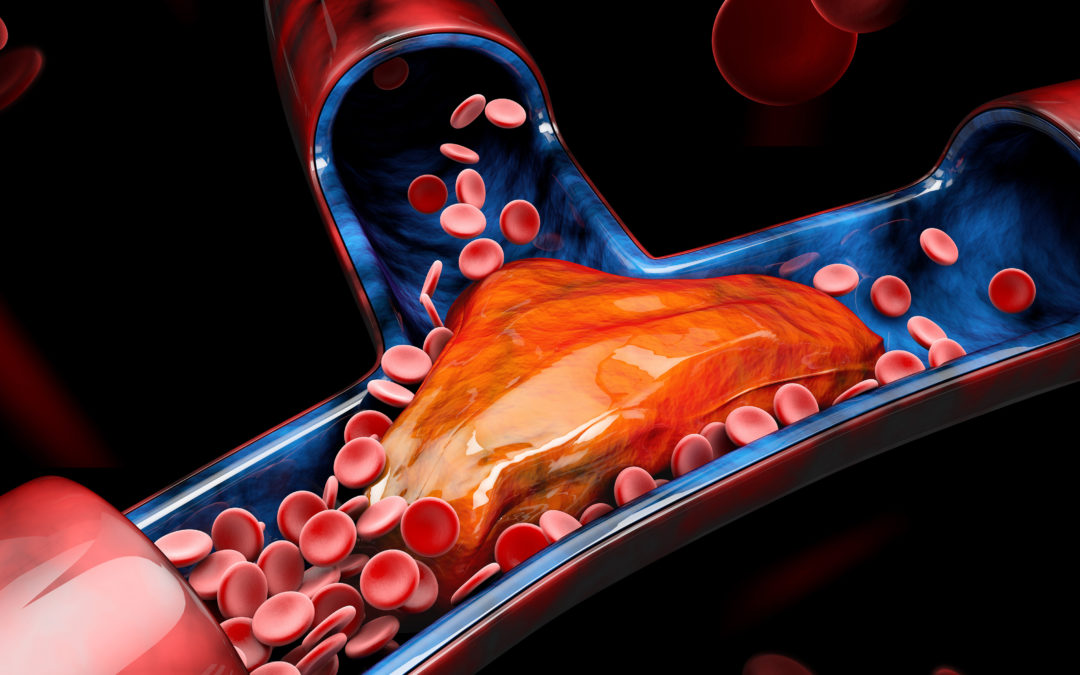
The body’s venous system is made up of veins with a series of valves inside them to keep the blood flowing in one direction, back to the heart. When the walls of the veins are damaged, blood can collect, and when the muscles relax flow in a retrograde manner which builds pressure within the venous system, further damaging the veins and, in some instances, causing the formation of blood clots. Over time this leads to vein disease.
The Stages of Vein Disease
As with many diseases, there are stages to vein disease.
Early Stages
The common early-stage symptoms of vein disease include:
- Spider Veins: Wispy red or purplish superficial veins visible like tangled webs on the skin.
- Varicose Veins: Unsightly twisted and bulging veins. They can often cause leg pain, swelling, itching, restlessness, and heaviness. Around 15% of the US population suffers from varicose veins.
Later Stages
The common late-stage symptoms of vein disease include:
- Skin Changes and Swelling: If the venous system is not working properly and the blood begins pooling, legs will often swell, especially around the ankles. The pooled blood will also cause the skin to take on a red or pale color.
- Venous Leg Ulcers: As the blood is not flowing as it should, the skin does not receive the nutrients it needs to heal wounds, which leads to an ulcer. Over time ulcers can become debilitating, painful, and infected.
When to Act
When vein disease is not treated, there is a flow-on effect that can damage the lymphatic system, which ultimately results in the accumulation of lipid, one of the causative factors in damage to vein walls.
The best time to act is when you first notice the symptoms of vein disease. Acting earlier helps to reign the disease in and minimize the likelihood of the disease progressing.
Treatment Options
A range of different treatment options are available, including:
- Compression stockings to stabilize weakened veins and keep blood flowing.
- Antibiotics can be prescribed to counter infection and anti-inflammatories to relieve inflammation.
- Sclerotherapy involves injections into the problematic veins that reroute the blood to healthy veins.
- Endovenous thermal ablation uses heat generated by a laser or high-frequency radio waves to stop blood flow through the problematic vein.
- Surgical ligation and removal involve tying off of the problematic vein before removing it.
Although the early stages of vein disease can appear relatively innocuous, it is important to act sooner rather than later. This will result in the best outcomes and increase the likelihood that the disease will not progress to the more serious stages.
by Lexington Vein Institute | May 3, 2021 | Blog, Leg Ulcers
Venous ulcers affect around 2% of Americans 65 and older and around 1% of the total population.
What are venous ulcers?
They are open sores that develop when the veins in the legs are not pushing the blood back up to your heart like they normally would. Blood backs up and pressure builds in the veins.
When this condition is left untreated, the increased pressure and excess fluid can cause an open sore. These slow-to-heal wounds usually occur on the leg, above the ankle.
Looking for information on venous ulcer risk? Who is at risk depends on a number of factors. Keep reading to learn more about who is most at risk of venous ulcers.
What Causes Venous Ulcers?
Weak valves and scarred and blocked veins cause the veins to malfunction. This is the underlying condition causing the backward flow of blood that ultimately leads to a lack of nutrients, dead cells, and damaged tissue that turns into this type of open wound.
Who is at Risk? Risk Assessment
There are many risk factors, but age and gender also play a part. As we get older, our veins lose elasticity and the valves in the veins become weak. Both of these affect the ability of the veins to control blood flow.
Females have a higher chance of developing this condition especially those over age 50.
Other risk factors include:
- Previous leg injury like muscle damage, burns, fracture of a long leg bone
- History of blood clots in the legs known as deep vein thrombosis
- Being tall
- Obesity
- Smoking
- Pregnancy
- Standing or sitting for long periods of time
- Family history of vein problems
- Blockage in the lymph vessels
- Varicose veins
What Changes Can You Make to Lower Your Risk?
Changing to and sticking with a healthy lifestyle can help you offset your risk factors. Don’t smoke or quit if you are a smoker. Adopt a healthy diet and get regular exercise.
If you have high blood pressure or diabetes, follow doctor’s orders to keep them under control. If you are overweight or obese, do what you can to get to your ideal weight.
Eventually, if your job requires you to sit for long periods of time, take breaks and move around. The same goes for standing too long. Give your legs a break from time to time.
Wearing compression socks can help to prevent blood from pooling in your legs.
Medical Professionals Guide to Venous Ulcers
Now that you know who is at risk for venous ulcers, you can take precautions and lower your risk by following a healthy diet and lifestyle especially if you have a family history of this condition. Speak to a professional to learn more about what you can do to avoid venous ulcers.
We at Lexington Vein Institute will address the source of your vein problem and help you produce an overall healthier vascular system to lower your risk for vein issues. Contact us today with questions or to schedule an appointment.

by Lexington Vein Institute | May 3, 2021 | Blog, Edema
Do you have swollen ankles?
If you do, you’ll know how annoying they can be! From struggling to get into your favorite shoes to the discomfort you can experience, it’s definitely not a fun experience.
But where did they come from? Why is everyone else walking around with totally normal ankles while yours are completely swollen?
Take a look at this guide looking at the causes of swelling and how you can treat them.
Edema Swelling
Edema is a condition in which fluid builds up in the tissues in your body. This eventually can cause swelling in certain areas, including your ankles and feet! Other spots that can be affected include your hands and legs.
Luckily, it can be treated. At Lexington Vein Institute, we have edema specialists who can evaluate your condition and find the right treatment for it, so you don’t have to live with swollen ankles forever.
Pregnancy Side Effect
When it comes to what causes swelling, pregnancy is one of the main causes. If you’re pregnant and have swollen feet and ankles, or even a swollen lower body, don’t be surprised!
Usually, this isn’t a cause for concern. However, if you’re seeing sudden swelling or it’s accompanied by pain, you should see a medical professional straight away. You could have preeclampsia, which is a condition where you have high blood pressure and protein is present in the urine.
Foot or Ankle Injury
Injuries often cause swelling, and an injury to the foot or ankle is no different! The most common injury that causes swelling is a sprained ankle, which isn’t a cause for concern. To reduce the swelling and heal, try to avoid walking on it and wrap the foot and ankle in a compression bandage.
If you have severe pain and swelling that doesn’t go away with rest, see a medical professional.
Lymphedema
Lymphedema is caused by a build-up of lymphatic fluid in your tissue, and it’s actually a cause of edema! It occurs when you’ve experienced issues with your lymph vessels or you’ve had your lymph nodes removed, and if left untreated it can cause further issues. Again, this is something we can diagnose and treat at the Lexington Vein Institute, so if you think you may have it then come in as soon as possible.
Blood Clots
If you’ve got a blood clot in your leg, it could be preventing blood from returning from your foot and back to the heart, causing your foot and ankle to swell. These can be life-threatening, so make sure to take it seriously if you have a swollen ankle for no apparent reason and see a medical professional. Signs of a blood clot include:
- Swelling in one leg
- A fever
- Pain
Get Help With Your Swollen Ankles
If you think edema is causing your swollen ankles, you don’t have to just put up with them! Visit us at the Lexington Vein Institute for professional, experienced treatment. If you have any questions, be sure to get in touch with our team; we’re always happy to help.

by Lexington Vein Institute | Mar 30, 2021 | Blog, Varicose Veins
There are many discussions around treatments for varicose veins, and most of them don’t work. The average American adult sits for 6 and a half hours every day. Causing blood circulation to slow down and increasing your chances of developing varicose veins.
There’s a simple activity you can do to improve blood circulation in your legs and help your varicose veins: elevating your legs!
Keep reading to learn exactly why elevating your legs helps with varicose veins.
We Can Thank Gravity
When you elevate your legs, you’re improving the circulation in your legs, and you get your blood moving in the right direction. Elevate your legs above your heart to give the veins the ability to counteract gravity. This will help the blood drain away from the veins, and you should notice a reduction in swelling and pain.
We can also thank gravity because elevating your legs reduces the pressure that gets built in your legs. To achieve the best results, raise your legs six to twelve inches higher than your heart and lay down in a comfortable position. Put pillows all down your legs and feet to support your legs in the right position comfortably.
Try to do this three to four times a day for around 15 minutes, and always wear loose-fitting clothing to ensure the best results. If your clothes are too tight, it’s not going to improve blood circulation at all and will instead compress your veins, causing more pain.
How to Incorporate Elevating Your Legs Into Your Schedule
Not only does elevating your legs during the day help with varicose veins, but it’s also good for your health. It’s recommended to walk away from your desk and computer screen for five minutes every hour.
This break is the perfect time to find a spot to lay and elevate your legs. Although it’s recommended to elevate your legs for 15 minutes at a time, even a little bit of relief is worth it during the day. On days that you’re not working,g be sure to follow all of the suggestions to achieve the best results.
When to Know When to See a Specialist
If your veins have changed color or are bulging, then you need to see a specialist. Also, if you’re experiencing a lot of pain and there doesn’t seem to be any relief, it’s time for you to see a specialist.
Take a look at these before and afters; if your veins start to look like the before photos, know that there is help available for you.
Treat Varicose Veins Today
Now that you know why elevating your legs helps be sure to include it in your daily routine!
If you’re ready to get rid of painful varicose veins, contact us and set up an appointment. Dr. Fadi Bacha, MD, is an expert in vein health and can’t wait to help you.