One in three Americans over the age of 45 have some form of vein disease. Many are unaware, while others view the symptoms as minor; however, vein disease must be taken seriously due to the veins’ integral role in blood supply and flow.
What is Vein Disease
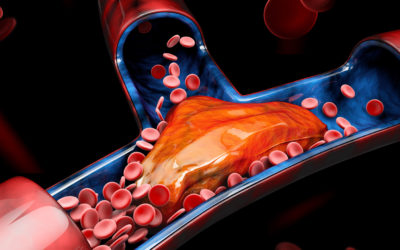
The body’s venous system is made up of veins with a series of valves inside them to keep the blood flowing in one direction, back to the heart. When the walls of the veins are damaged, blood can collect, and when the muscles relax flow in a retrograde manner which builds pressure within the venous system, further damaging the veins and, in some instances, causing the formation of blood clots. Over time this leads to vein disease.
The Stages of Vein Disease
As with many diseases, there are stages to vein disease.
Early Stages
The common early-stage symptoms of vein disease include:
- Spider Veins: Wispy red or purplish superficial veins visible like tangled webs on the skin.
- Varicose Veins: Unsightly twisted and bulging veins. They can often cause leg pain, swelling, itching, restlessness, and heaviness. Around 15% of the US population suffers from varicose veins.
Later Stages
The common late-stage symptoms of vein disease include:
- Skin Changes and Swelling: If the venous system is not working properly and the blood begins pooling, legs will often swell, especially around the ankles. The pooled blood will also cause the skin to take on a red or pale color.
- Venous Leg Ulcers: As the blood is not flowing as it should, the skin does not receive the nutrients it needs to heal wounds, which leads to an ulcer. Over time ulcers can become debilitating, painful, and infected.
When to Act
When vein disease is not treated, there is a flow-on effect that can damage the lymphatic system, which ultimately results in the accumulation of lipid, one of the causative factors in damage to vein walls.
The best time to act is when you first notice the symptoms of vein disease. Acting earlier helps to reign the disease in and minimize the likelihood of the disease progressing.
Treatment Options
A range of different treatment options are available, including:
- Compression stockings to stabilize weakened veins and keep blood flowing.
- Antibiotics can be prescribed to counter infection and anti-inflammatories to relieve inflammation.
- Sclerotherapy involves injections into the problematic veins that reroute the blood to healthy veins.
- Endovenous thermal ablation uses heat generated by a laser or high-frequency radio waves to stop blood flow through the problematic vein.
- Surgical ligation and removal involve tying off of the problematic vein before removing it.
Although the early stages of vein disease can appear relatively innocuous, it is important to act sooner rather than later. This will result in the best outcomes and increase the likelihood that the disease will not progress to the more serious stages.